|
The North American Menopause Society (N.A.M.S.) Menopausal Model
Why the North American Menopause Society (NAMS) Model Inhibits Proper Patient Evaluation The cornerstone of the North American Menopause Society course on menopausal management begins with a definition of menopause. According to N.A.M.S., menopause is defined as “ ..12 months of amenorrhea following the final menstrual period (FMP), which reflects a near complete but natural diminution of ovarian hormone secretion. Menopause means the end of natural childbearing (without assisted reproductive techniques). There is no adequate independent biological marker for menopause.”
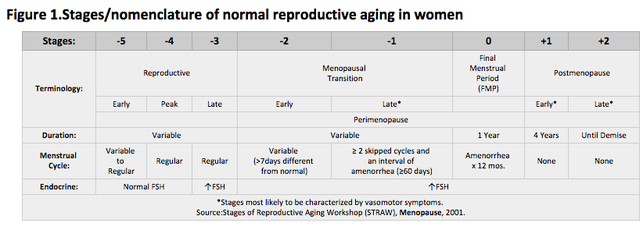
Below is a table breaking down a woman’s reproductive life into various stages, with the final period as the anchor point of the table. |
|
It is easy to see that no endocrinologic criteria is listed. All the stages are clinical.
What is wrong with this model? If I were to see a thirty-year-old patient who had gone twelve months without a period, I would not assume this represents early menopause. I would begin with an endocrine work up and delve into what is happening to the hypothalamus, pituitary, ovaries, and uterus. If the answer was still unclear, I would evaluate prolactin, thyroid function and adrenal function as well as nutritional status, exercise and any current medications. Just because a woman is forty-five or fifty-years-old and is complaining of hot flashes, does not mean that her ovaries are no longer making hormones. In the past three years, I have done lab work for over two thousand women with hormonal issues. I still become surprised and learn new things every day. I see women in their thirties with very high FSH and virtually no estrogen, progesterone or testosterone. I also see fifty-year-old women with moderately elevated FSH but elevated estradiol and estrone, no progesterone and normal testosterone. Every day I see menopausal women with high and low testosterone. Some doctors have claimed that laboratory tests for determining total testosterone is inaccurate. Why should that be the case? Laboratory testing is automated and is very accurate. Sometimes we do not understand the results—that is no reason to blame the lab. Every day I see women who had a hysterectomy with the ovaries intact. When they start getting hot flashes, many doctors put them on estrogen only and they are miserable. Many of these women already have too much estrogen. If they still had a uterus, they would be experiencing heavy bleeding along with the hot flashes. Adding additional estrogen only makes them feel worse. When I took the N.A.M.S. Menopausal Management Certification Review Course in 2003, we were instructed not to order FSH or estradiol levels. It would just confuse us. I did not take their advice as I wanted to learn as much as I could about my patients. Two months later, I learned about compounding pharmacies and bioidentical hormones. How was it possible that I had just become certified by the most prestigious menopausal organization in the nation, and they never mentioned the existence of bioidentical hormones? It was never pointed out that I could replace depleted hormones with an identical molecule, one that could be measured, allowing me to treat female hormone abnormalities like a real doctor. Run a history and physical. Measure hormones from the whole system; top to bottom. Find out what the problem is. Replace what is needed with the identical molecule. Retest (repeating appropriate patient histories and physicals) to evaluate your progress and to determine how the patient is feeling. So, what is to be done? We must learn new things and manage menopause and irregular bleeding states for the endocrinologic problems that arise. We need to understand the physiology, learn what is normal and appreciate that each woman, each patient, is an individual. Each woman handles hormones in their own unique way -- there is no single magic solution. Today’s leaders in menopausal management are our patients. If our therapies aren’t working for them, they tell us. If we don’t listen, they will find another doctor. They read books. They go to the Internet. They talk to friends. We, the professionals, must do the same. If a patient brings me a book, I read it. For professional sources, my bible is Speroff and Fritz, Clinical Gynecologic Endocrinology and Infertility -- it must be the latest edition (Seventh Edition). There have been great advances since the Sixth Edition, especially in understanding the relationship between insulin and female hormones. Most of the books on bioidentical hormones are written for lay people. Some contain excellent information while others, not so much. I am constantly reading—even the less than perfect books provide some interesting insights. I want to share what I have learned and will be building this website as a teaching and learning tool. There is a better way then what we have been taught up to now—a way of viewing the gradual changes in a woman’s hormone status based on the physiology. There are many therapies using bioidentical hormones to act like natural hormones and can be monitored using standard laboratory testing. Take a deep breath. It will be OK. There is a lot to learn. The results in your patients will surprise you. |